In recent years, the mental health of PhD students has garnered significant attention, with calls for urgent policy interventions to address what some describe as a ‘mental health crisis’ in higher education (Evans et al. 2018). Concerns over depression, anxiety, and even suicidal ideation have prompted universities and governments to consider how the pressures of doctoral education may be contributing to these outcomes. Reports from the Council of Graduate Schools (2021) and others have highlighted mental health as a critical issue (Forrester 2021, Woolston 2017). But how severe are these issues, and are they truly unique to PhD programmes?
Existing research has relied largely on cross-sectional surveys, often based on small, non-representative samples with inadequate benchmarks. Additionally, despite the stigma around mental health issues (Mallesh et al. 2015), these surveys tend to overestimate their prevalence (Levis et al. 2020). This overestimation, combined with the absence of longitudinal data and proper benchmarks, weakens the ability to accurately assess mental health and the impact of doctoral studies. Together with Dagmar Müller, we turn to administrative data from Sweden to address these gaps and provide a more rigorous, comprehensive analysis of the mental health challenges faced by PhD students (Keloharju et al. 2024).
Reassessing the mental health crisis in graduate education
Our study uses medically validated data to assess mental health conditions among PhD students in Sweden, focusing on depression, anxiety, and suicide rates. We compare these outcomes with two key benchmarks: Master’s graduates who did not pursue a PhD and the general population. Importantly, our longitudinal approach allows us to track the mental health of PhD students both before and after entering their programmes, offering insights into whether doctoral studies themselves are a contributing factor to mental health deterioration.
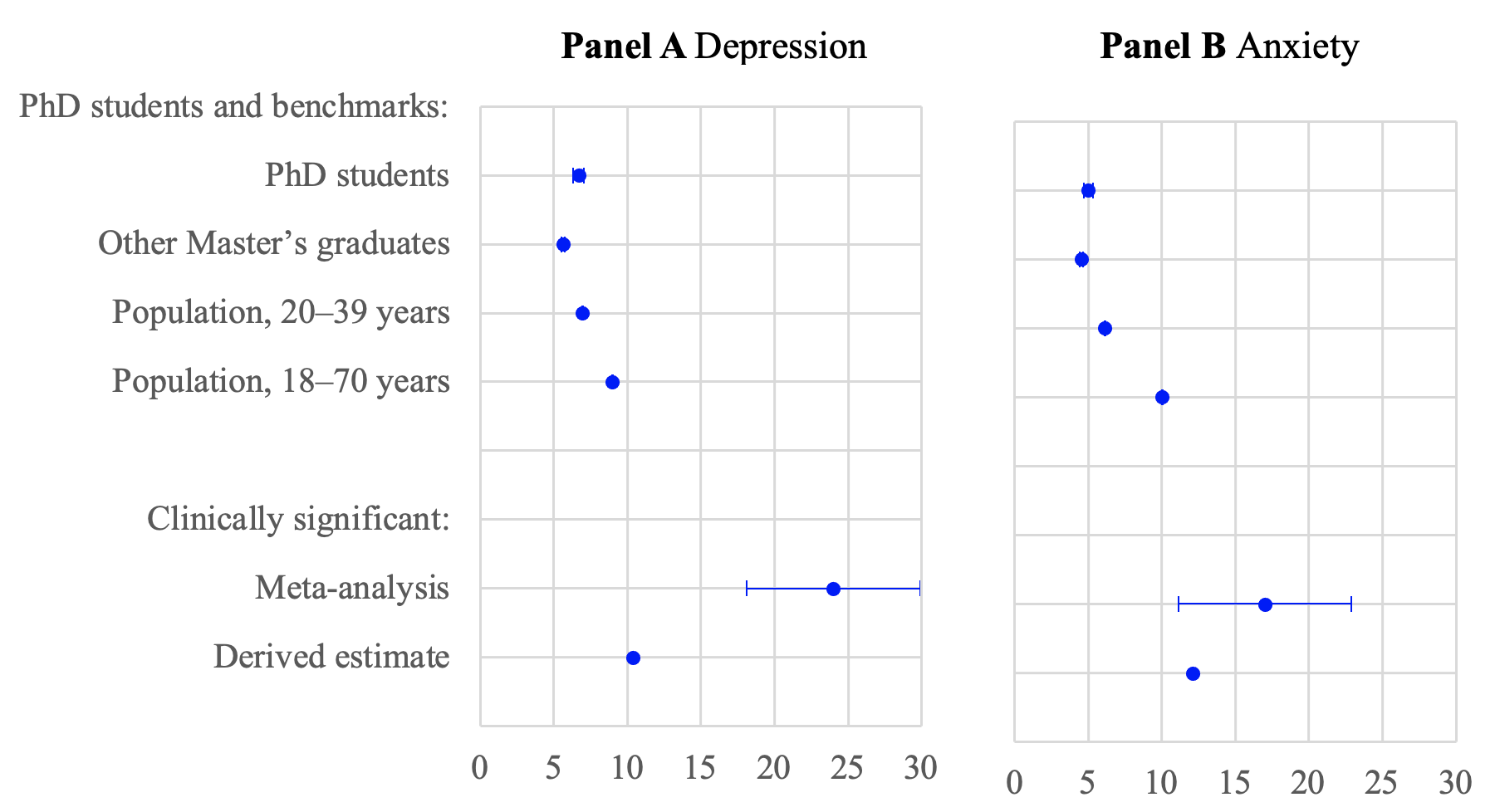
Our findings, displayed in Figure 1, challenge the prevailing view that PhD students face a disproportionately high risk of mental health problems. While previous studies such as the meta-analysis by Satinsky et al. (2021) suggest that up to 24% of PhD students experience clinically significant depression, our data indicate a much lower prevalence. Specifically, we find that only 6.7% of Swedish PhD students receive treatment for depression in a given year. After adjusting for methodological differences, we estimate that the depression rate, shown as ‘derived estimate’ in Figure 1, comprises no more than 43% of the Satinsky et al. (2021) meta-estimate of 24%. We also observe lower rates of anxiety and completed suicides than earlier studies. For instance, while prior research reports suicidal ideation in PhD students above 10%, our findings indicate that these thoughts almost never lead to completed suicides. This aligns with Deaton and Case (2015), who highlight the weak link between self-reported distress and suicide rates. Overall, these results suggest that graduate studies may be less harmful to mental health than previously feared.
Figure 1 Annual prevalence of depression and anxiety among PhD students and benchmarks
Comparing PhD students to their peers
To better understand mental health dynamics within the PhD population, we compared their outcomes with those of Master’s graduates. We found that the prevalence of depression among Swedish PhD students is 1.1 percentage points higher than it is among their peers who did not pursue doctoral studies. This difference suggests that while mental health concerns are present, they may not be as acute as often portrayed in the media and in academic reports.
Furthermore, the overall rate of depression among PhD students aligns closely with the rate observed in the general population aged 20–39. Anxiety follows a similar pattern, with only a marginally higher prevalence among PhD students compared to their non-PhD counterparts. These findings call into question the notion that PhD programmes are a unique driver of mental health problems and suggest that broader societal factors may play a larger role.
Is the PhD programme to blame?
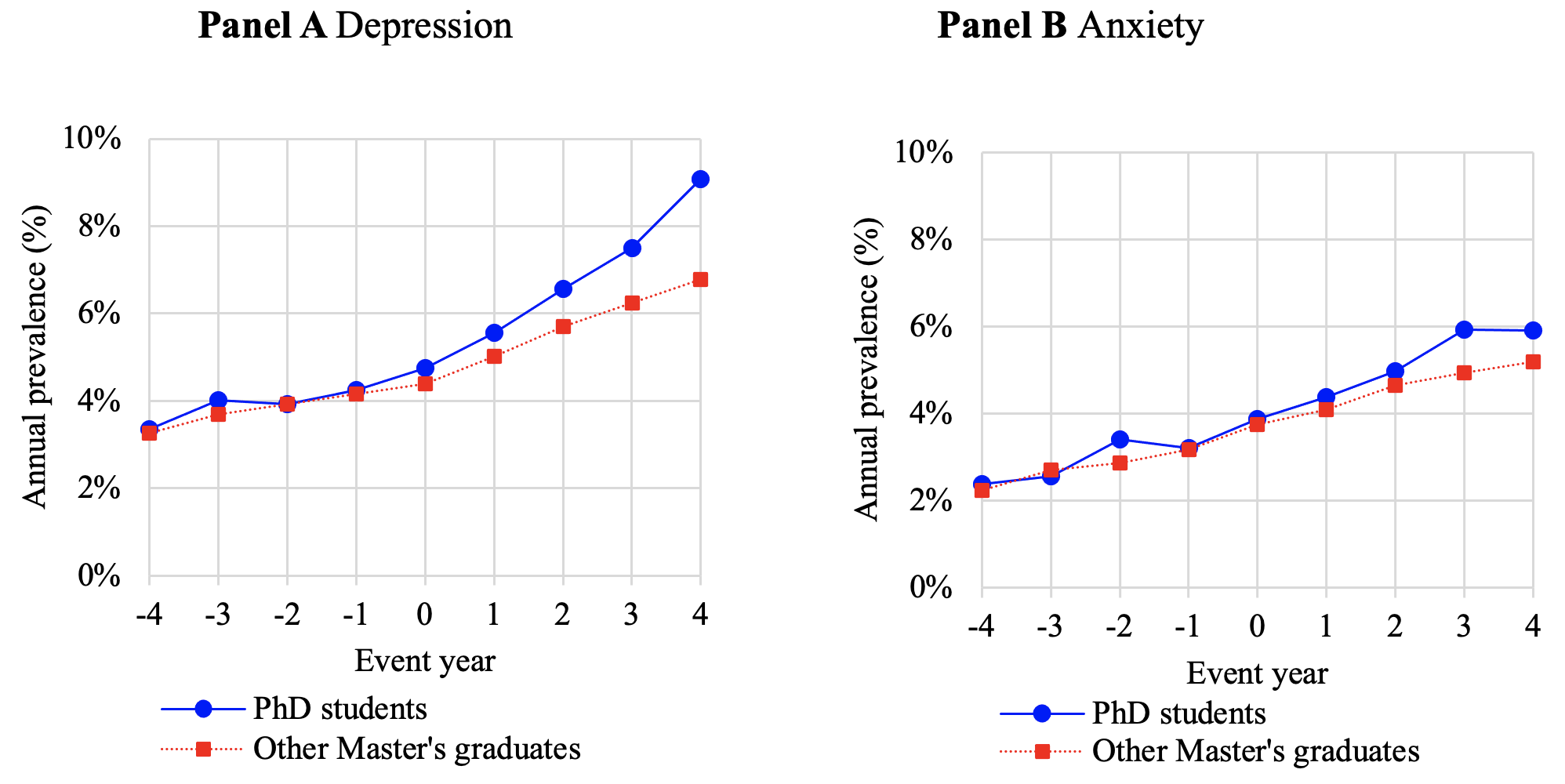
Our longitudinal analysis offers an important insight: as displayed in Figure 2, the disparity in mental health between PhD students and their peers emerges only after they begin their doctoral studies. This suggests that some aspects of the PhD experience – such as academic environment, expectations, or work culture – may indeed contribute to worsening mental health. Using difference-in-differences methods, we also estimate that the onset of depression during PhD programmes accounts for nearly all of the difference between PhD students and Master’s graduates once we have accounted for gender, age, high school GPA, and indicators for parental anxiety and depression.
Figure 2 Development of mental health over time for PhD students and control group
International students: A different picture
Another intriguing aspect of our research is the mental health disparity between Swedish and international PhD students. We find that foreign students exhibit significantly lower rates of depression and anxiety, with only 2% receiving treatment compared to 5–7% for Swedish students. This could be due to self-selection, with more resilient individuals enrolling in international programmes, or to underreporting, as international students may be less familiar with the Swedish healthcare system. The added pressures of adapting to a new culture, navigating different academic expectations, and establishing social support networks are likely stressors, yet these students appear less likely to report or seek treatment for mental health issues.
This raises important policy questions: are international students underreporting their mental health struggles due to barriers in accessing local healthcare services, or are they genuinely less affected? Universities need to ensure that mental health support systems are accessible to all students, regardless of nationality. Creating more culturally sensitive support structures, increasing outreach, and ensuring that international students are well-informed about available mental health services should be a priority for institutions hosting foreign students.
Implications for policy and practice
Our findings have important implications for policymakers and university administrators. While mental health concerns among PhD students are real, they may not be as severe or widespread as previously thought. This more nuanced understanding of the issue should guide future interventions. Universities ought to focus on providing targeted support for students during the most stressful phases of their doctoral programmes, rather than assuming that the entire PhD experience is inherently harmful to mental health.
Additionally, our use of administrative data provides a model for future research. By moving beyond small surveys to incorporate large-scale, longitudinal data, researchers can offer more accurate assessments of the mental health challenges in academia. This approach not only strengthens the evidence base but also provides policymakers with the information they need to design effective interventions. Furthermore, universities might consider offering stress management and mental health resources specifically tailored to the PhD experience, addressing both the academic and personal challenges faced by students.
Conclusion
In conclusion, while the mental health of PhD students is a legitimate concern, the widespread notion of a ‘mental health crisis’ may be overstated. Our research shows that PhD students in Sweden are not significantly more vulnerable to depression or anxiety than their peers or the general population. Moreover, the disparities that do exist appear to develop during the PhD programme itself, suggesting that targeted interventions at specific stages of doctoral training may be more effective than broad-based policies. By adopting a more data-driven approach, universities and policymakers can better support the mental well-being of PhD students, ensuring they thrive both academically and personally.
References
Council of Graduate Schools and the Jed Foundation (2024), Supporting Graduate Student Mental Health and Well-being, Washington, DC.
Deaton, A and A Case (2015), “Suicide and happiness”, VoxEU.org, 18 July.
Evans, T M, B Lindsay, J Beltran Gastelum, L Todd Weiss and N L Vanderford (2018), “Evidence for a mental health crisis in graduate education”, Nature Biotechnology 36: 282–84.
Forrester, N (2021), “Mental health of graduate students sorely overlooked”, Nature 595: 135–37.
Keloharju, M, S Knüpfer, D Müller and J Tåg (2024), “PhD studies hurt mental health, but less than previously feared”, Research Policy 53(8): 105078.
Levis, B, A Benedetti, J P Ioannidis, Y Sun, Z Negeri, C He, Y Wu, A Krishnan, P M Bhandari, D Neupane and M Imran (2020), “Patient Health Questionnaire-9 scores do not accurately estimate depression prevalence: Individual participant data meta-analysis”, Journal of Clinical Epidemiology 122: 115–28.
Mallesh, P, A Suziedelyte and P Bharadwaj (2015), “Mental health stigma”, VoxEU.org, 3 July.
Satinsky, E N, T Kimura, M V Kiang, R Abebe, S Cunningham, H Lee, X Lin, C H Liu, I Rudan, S Sen and M Tomlinson (2021), “Systematic review and meta-analysis of depression, anxiety, and suicidal ideation among Ph.D. students”, Scientific Reports 11: 14370.
Woolston, C (2017), “Graduate survey: A love–hurt relationship”, Nature 550: 549–52.